Best Sleeping Position For IT Band Pain (2025)
Updated: March 31, 2025 | Published: July 2, 2024There’s nothing worse than trying to move when our bodies hurt. The IT (iliotibial) band is a length of connective tissue running from your outer hip to just below your knee. Activities that require repeated knee flexion, like walking and running, can irritate and inflame the IT band (Hadeed et al., 2023). The result: IT band pain.
If you’re experiencing IT band pain, one of the simplest and best ways to treat it is to get a good night’s sleep (Mousavi et al., 2021). In this article, we’ll explain the best sleeping positions for IT band pain so you can get back to your normal routine as quickly as possible.
Disclaimer: We co-authored this article with dedicated healthcare provider Dr. Gregory Stoltz, DC. The following tips, including those from Dr. Stoltz, are general recommendations and aren’t meant to replace your doctor’s professional diagnosis. Always consult your physician before trying these sleep positions at home.
1. Sleeping on your back
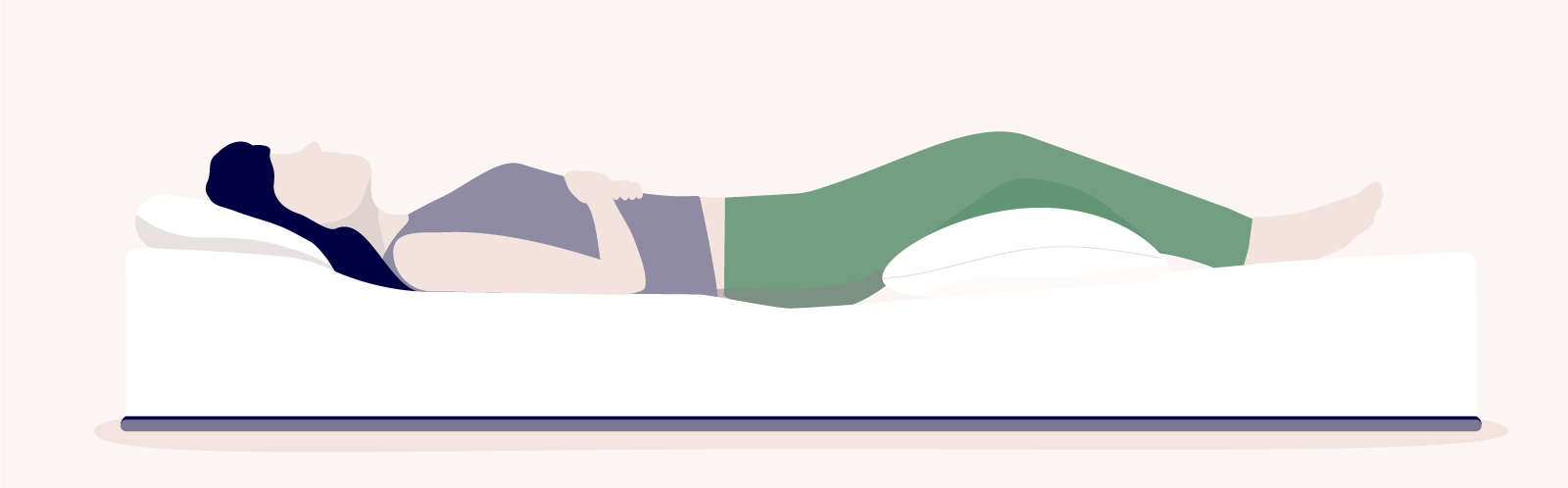
The best sleeping position for IT band pain is flat on your back. Sleeping on your back with your legs extended will distribute your weight evenly across the surface of your bed. This prevents you from putting extra pressure on your hip or knees.
A great tip to decrease IT band pain is to elevate your legs with a pillow beneath the affected knee. Staying in a relatively still position—like when you’re asleep—can cause your muscles to constrict and apply pressure to the IT band.
Keeping your leg elevated not only helps prevent the IT band from tensing up, but also promotes better circulation. This helps if you struggle with peripheral artery disease (PAD).
If you’re not used to sleeping on your back, you might find this position uncomfortable, especially if you have pre-existing back pain. The right kind of mattress can help with that, especially if it has pressure-point-relieving features and zoned body support.
READ MORE: Get our ranked list of the best mattresses for back pain
You can also consider investing in a bed with an adjustable base, like the Octave Adjustable Bed. With an adjustable bed, you can control the elevation of specific areas of your mattress. It’s easy to customize your bed’s elevation to your comfort level and keep your legs at that elevation all night.
2. Sleeping on your side
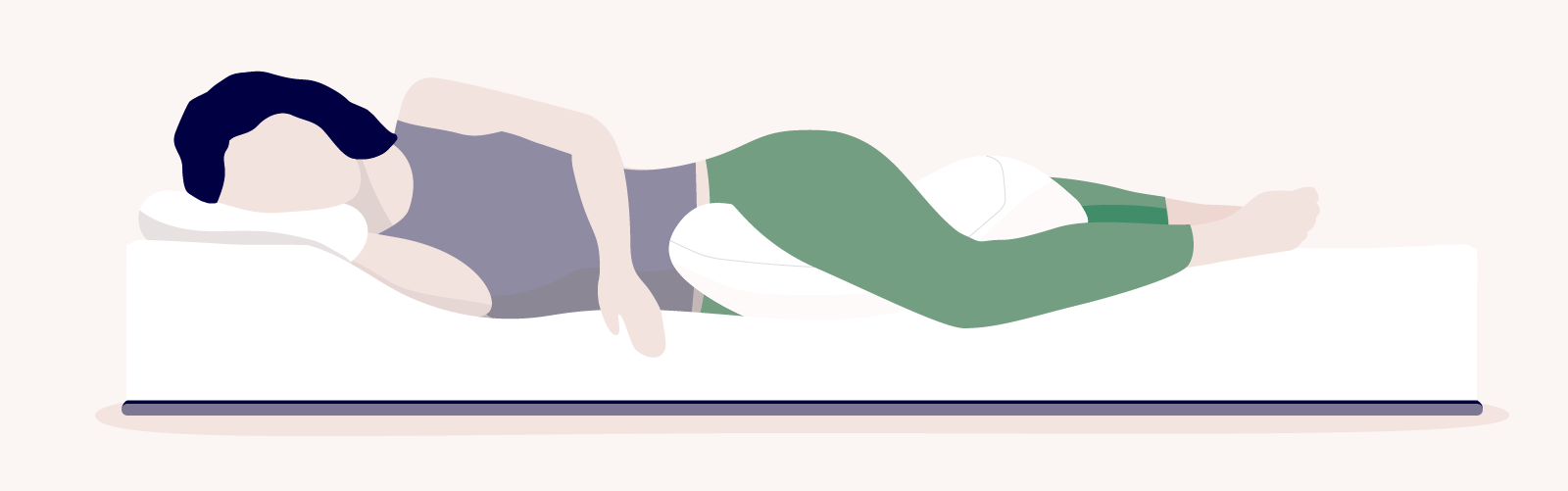
If you have IT band pain and prefer sleeping on your side, you can still do so—as long as you sleep on your unaffected side and keep your spine aligned.
Try to elevate your affected leg by sleeping with a pillow between your knees. Use a pillow that’s thick enough to keep your knee elevated to the height of your hips. Just like when sleeping on your back, you should also keep your legs comfortably extended.
Your hips should also be aligned so that they’re vertically “stacked” over each other. Your shoulders should be stacked, too. This will relieve the most pressure from the affected area and stop you from straining your joints while you’re asleep. This position may also help if you’re struggling with lower back pain.
READ MORE: What’s the best sleeping position for lower back pain?
Keep in mind that sleeping on your side is only a good idea if you’re dealing with IT band pain in just one of your legs. If you’re experiencing pain in both legs, sleeping on your side may not be your best option to get a deep restful sleep.
When you sleep on an area that’s sore, your body unconsciously tries to relieve that pressure while you sleep. This can cause you to toss and turn more often, diminishing the quality of your sleep.
Find it hard to sleep on your side? Consider switching to a mattress that’s designed for side sleepers. Octave mattresses offer zoned ergonomic support, helping to eliminate pressure points and keep your spine in proper alignment while you sleep, making them some of our best mattresses for side sleepers.
Tips for sleeping better with IT band pain
Bending and straightening your leg rubs the IT band against your femur. While bending the knee is normal, pain is not. Repeatedly doing activities that cause the knee to bend can create friction around the IT band, which leads to irritation and inflammation.
This causes intense pain in your lower knee that often gets worse the more active you are—the telltale sign of IT band pain. With proper treatment, however, IT band pain usually disappears in about 4–8 weeks.
The following sleep tips can also help you find your way back to your normal pain-free self (Kane et al., 2019):
- Avoid strenuous physical activity throughout the day. Try not to do anything physically challenging, even if it’s something that doesn’t involve your legs. This reduces the chance that you’ll fall asleep with tensed-up leg muscles, which in turn relieves pressure on the IT band.
- Stretch before going to sleep. Certain stretches, like the Piriformis stretch, can help. Start by lying on your back, keeping your legs straight. Lift your affected leg and bend your knee. With your opposite hand, reach over and gently pull your knee toward your opposite shoulder. Hold for 15–30 seconds. Repeat this stretch 2–4 times.
- Avoid caffeine or alcohol before bedtime. You probably know that caffeine before bed is a bad idea, but so is alcohol. Caffeine makes it more difficult for you to fall asleep in the first place. And alcohol makes it much harder for your body to achieve REM sleep, which is when you sleep the most deeply. Deep sleep will help you heal faster.
- Massage the muscles around the affected area. If a professional massage therapist isn’t an option, you can also self-massage the affected muscles in your legs. Lay a foam roller (or even a pool noodle) on the ground and lie sideways on top of it. Roll back and forth slowly from your hip to your knee, making sure to massage your entire IT band.
- Invest in a good mattress. If you’re dealing with IT band pain on a long-term basis, think about what type of mattress works best for you, no matter what your preferred sleep style is. A change in bed can make all the difference.
- Ice the affected area. IT band pain is the result of inflammation. Just like other kinds of swelling, applying something cold can help to treat it. Gently press an ice pack or a cold compress against your knee every 15 minutes for 2–3 hours before you go to sleep. This can reduce pain considerably. Remember not to apply ice directly against your skin.
- Treat your pain with over-the-counter anti-inflammatory medication. If your doctor recommends it, non-steroidal anti-inflammatory drugs (NSAIDs) like Advil (ibuprofen) can help to reduce pain and swelling. Alternatives like Tylenol (acetaminophen) can also help to reduce pain, but may not reduce inflammation. Always check with your doctor before taking pain medication.
READ MORE: Check out our ranked list of the best mattresses for scoliosis
Our goal is to provide the information you need to find the mattress that’s right for you. Get started with some of our most popular mattress shopping resources:
- Best Mattress Guides: Best Mattress Canada, Best Mattress In a Box
- Reviews: Douglas Original, Logan & Cove Choice, Juno, Octave Vista
- Comparisons: Douglas vs Endy, Douglas vs Casper
We use independent, third-party engineering firms (commissioned by us) with the APEGA stamp of approval to conduct mattress testing on our behalf, using publicly available data. We review and test all mattresses on 40+ criteria we think are important to you, including price, country of manufacture, sleep trial, warranty, features, materials used, motion isolation and edge support ratings, customer satisfaction reviews, returns, and refunds.
References:
- Andrew Hadeed, David C. Tapscott. “Iliotibial band friction Syndrome.” StatPearls – NCBI Bookshelf (May 23, 2023). https://www.ncbi.nlm.nih.gov/books/NBK542185/.
- Mousavi, Seyed Hamed, et al. “Factors Associated With Lower Limb Injuries in Recreational Runners: A Cross-Sectional Survey Including Mental Aspects and Sleep Quality.” Journal of Sports Science and Medicine, pp. 204–15 (March 2021). https://doi.org/10.52082/jssm.2021.204.
- Kane, Shawn F., et al. “Management of Chronic Tendon Injuries.” AAFP (August 1, 2019). https://www.aafp.org/pubs/afp/issues/2019/0801/p147.html.